I was called by a prospective patient today who was clearly confused about the recommendations she had gotten from her other doctors. This very nice woman from Fort Collins, Colorado has suffered headache pain for many years since a whiplash accident. This story is classic for chronic headache pain that can be treated with migraine surgery, also known as nerve decompression. Her neurosurgeon has recommended spinal surgery for her, but her doctor, nor as it turns out her neurosurgeon, likely understands the cause of her pain. It is likely that she needs PERIPHERAL nerve decompression rather than the NERVE ROOT decompression as her neurosurgeon has recommended. Let’s discuss the difference.
Nerves are the means by which a sensation gets from the skin or soft tissue to the brain. A PERIPHERAL nerve is found in the skin, muscle, and soft tissue of the body, and leads to a CENTRAL portion of the nerve, found in the spinal cord and brain. As it reaches the spinal cord, the peripheral nerve leads to a NERVE ROOT, which is the collection of nerves that runs through gaps in the spinal bones, or vertebra. These gaps are called foramen. The nerve root passes through the foramen before joining the spinal cord on the way to the brain.
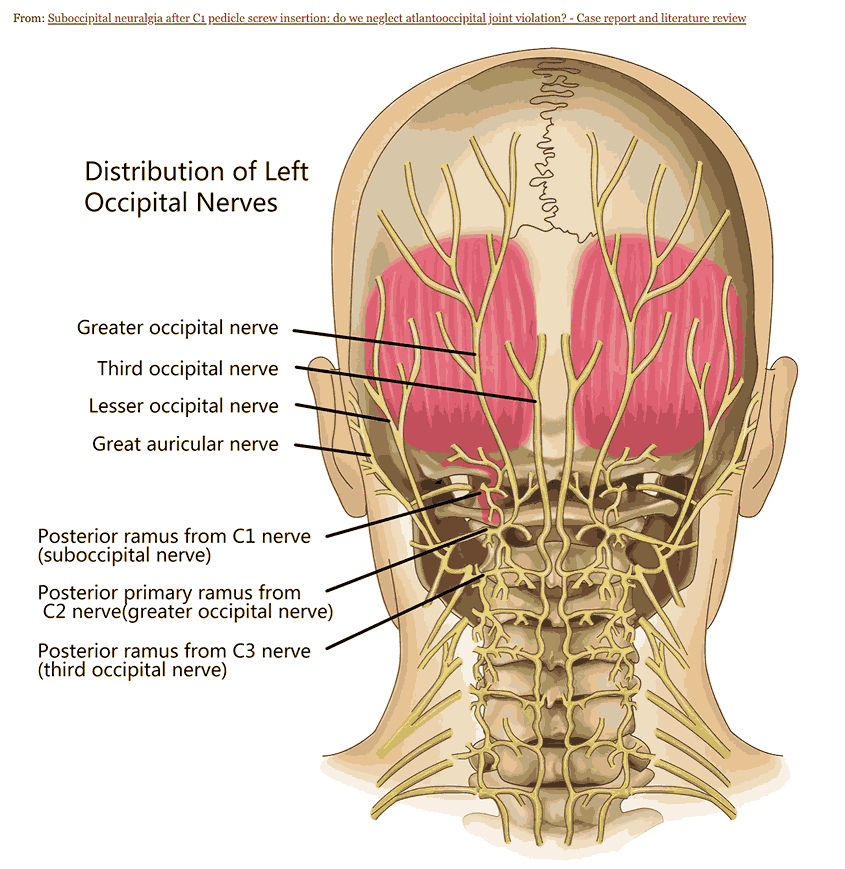
Now imagine a nerve, running from the back of the scalp, taking signals from the skin and muscle of the back of the head and neck to the brain. This nerve actually exists and is called the Greater Occipital Nerve (GON). On its way to the brain, the GON joins other nerves in the C2 nerve root (the nerve root that occupies the foramen at the second cervical vertebra.) As the nerves travel with the C2 nerve root through the foramen of the spine, they reach the spinal cord and then travel to the brain. On it’s way to the C2 nerve root, the GON passes through muscle and connective tissue of the back of the head and neck. This is the simple anatomy of the greater occipital nerve.
Now, let’s think of the GON as a 2 lane highway. (I need to give credit here to my friend and fellow migraine surgeon Dr. Ziv Peled who practices in the Bay Area, as this traffic analogy is originally his. This version is greatly expanded.) The nerve highway starts at the scalp and runs through muscles and connective tissue to the spinal cord to the brain. But there is construction on the road! The construction narrows the highway causing a back-up and distress of the cars, or in this case the nerve signals, passing through the nerve highway. From the construction point on, there is only one lane of traffic, and the drivers (or nerve signals in this case) are irritated and angry and distressed because of the constriction of their passage. When they get where they are going, the brain, they are irritating and create pain all around.

Spinal Surgery vs Migraine Surgery
So what matters here is WHERE the traffic is constricted to one lane. We need to know where the nerve highway is affected. So let’s expand on our metaphor. When we administer a nerve block, as we do to diagnose patients with peripheral nerve irritation, we are shutting down the nerve highway at a specific spot where the block is performed. Think of the nerve block as a bridge that is out or blocked- anything that happens on the far side of the bridge is not felt on the near side, or in the brain, because the irritated drivers never make it over the bridge block to create havoc at the destination.
But let’s take a patient like the one who called me, who has had a whiplash injury in the past. Let’s think about what happens when she sees the neurosurgeon. The whiplash or head trauma often causes chronic tightness in the neck at the base of the skull where the GON passes through several muscles that serve to stabilize the head and neck. In her case, the traffic is actually starting at the GON at the base of the skull. The C2 nerve block improves the pain by taking out the bridge at the entrance to the spinal cord- everything on the far side of the bridge is not felt because the irritated traffic is stopped at the bridge/nerve block. The neurosurgeon mistakenly assumes that the constriction is at the foramen where the nerve block was performed. So the neurosurgeon operates on the patient, loosening the foramen even though the problem is farther out at the muscles at the base of the skull. As the patient recovers, the pain is unchanged and the surgery is a failure because the attempt to alleviate the constriction was performed at the wrong spot.
The only way to tell where the traffic is ACTUALLY created, and where the nerve is really constricted, is to do a PERIPHERAL nerve block at the point that the GON goes through the muscle. If a nerve block in this spot is successful, we know that the C2 nerve root is not the issue. In blocking the bridge further away (distally) from the nerve root, we have stopped the distressed traffic only on the far side of the block. The traffic is apparently flowing fine at C2, at the near side of the blocked bridge, and the brain is still receiving normal flow through the proximal 2 lane highway. This tells us that the operation the patient requires is a PERIPHERAL nerve decompression to provide relief of the constricted traffic at the base of the skull and muscles of the neck rather than at the spine.
Now here is the test to see if we really understand things. If a nerve block at the GON does not work, but a block at the C2 nerve root does work, we then know that the problem is indeed at the nerve root and spinal surgery is indicated. If that last statement makes sense to you, then you understand the basis of peripheral nerve constriction vs. more central nerve constriction. We hope that you therefore understand when spinal surgery is indicated vs when migraine surgery, or peripheral nerve decompression, is indicated. Unfortunately, your understanding of this issue may be better than many spinal surgeon’s understanding when operating for headache pain.
Some neurosurgeons do understand this issue and screen properly to make sure that their diagnosis of spinal stenosis at the foramen is correct. Because I’ve seen so many patients who have had previous C-spine surgery and still have pain, it is clear that many patients are getting spinal surgery by doctors who don’t quite understand the nature of peripheral nerve compression.
I had this discussion with the patient I spoke with today, and now I’ve had this discussion with you. If you are unclear as to whether your doctor or neurosurgeon has a complete grasp on the cause of your headache pain, take the time to see a migraine surgeon who can clarify your diagnosis. If you are in the Los Angeles, Southern California, or Colorado regions, I am happy to see you in my offices there. Please call our patient coordinators at 805-969-9004 if you would like to make an in-person or virtual appointment to discuss your headaches. And please use online educational websites such as headachesurgery.com to familiarize yourself with migraine surgery, nerve decompression, and headache pain relief. Education and understanding are your best weapons against migraine and headache pain.